Quality improvement Theory
Healthcare organizations strive to provide the best possible care to patients, constantly seeking ways to improve their systems and processes. In this pursuit, quality improvement theory plays a crucial role. Quality improvement theory offers a systematic approach to enhance healthcare delivery, patient outcomes, and overall organizational performance. By understanding and implementing key concepts and principles of quality improvement theory, healthcare professionals can identify areas for improvement, drive changes, and optimize patient safety. This article explores the application of quality improvement theory in healthcare, highlighting its significance, key concepts, role in enhancing patient safety, implementation strategies, evaluation methods, challenges, successful case studies, and future directions. By delving into these aspects, we can gain insights into the effective utilization of quality improvement theory to drive positive change in healthcare settings.
1. Introduction to quality improvement theory in healthcare
Defining quality improvement theory
Quality improvement theory, in the context of healthcare, refers to a systematic approach used to enhance the quality and safety of patient care. It involves the application of various methodologies and strategies to identify areas for improvement, implement changes, and measure the impact of those changes.
The significance of quality improvement theory in healthcare
Quality improvement theory plays a vital role in healthcare as it enables healthcare organizations to deliver better outcomes, improve patient satisfaction, and reduce medical errors. By implementing evidence-based practices and continuously monitoring and evaluating processes, healthcare providers can identify gaps in care and implement targeted improvements to enhance the overall quality of healthcare services.
2. Key concepts and principles of quality improvement theory
Understanding the basic principles of quality improvement theory
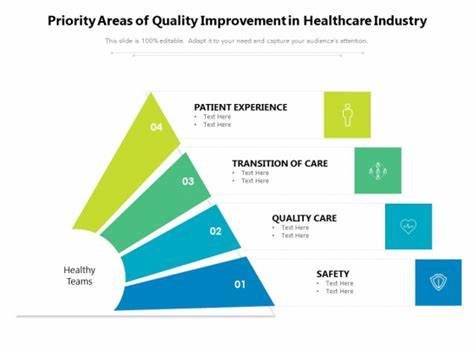
Quality improvement theory is built upon several key principles, including:
1. Patient-Centered Care: Placing the patient at the center of care and involving them in decision-making processes.
2. Continuous Improvement: Embracing a culture of continuous learning, innovation, and improvement.
3. Teamwork and Collaboration: Encouraging interdisciplinary collaboration and communication to foster effective teamwork.
4. Data-Driven Decision Making: Collecting and analyzing data to identify areas for improvement and guide decision-making.
5. Standardization: Implementing standardized processes and best practices to reduce variability and enhance reliability in care delivery.
Components of quality improvement theory
Quality improvement theory consists of several components, such as:
1. Define: Clearly articulating the problem or goal to be addressed.
2. Measure: Collecting relevant data to establish a baseline and monitor progress.
3. Analyze: Identifying root causes and barriers to improvement.
4. Improve: Implementing evidence-based changes and interventions.
5. Control: Monitoring and sustaining improvements over time.
3. The role of quality improvement theory in enhancing patient safety
Link between quality improvement theory and patient safety
Quality improvement theory is closely linked to patient safety, as its principles and methodologies aim to identify and mitigate risks to patient well-being. By promoting a culture of safety, implementing evidence-based practices, and actively involving patients and healthcare providers in identifying potential hazards, quality improvement theory contributes to reducing medical errors and improving patient outcomes.
Methods for integrating quality improvement theory to enhance patient safety
Integrating quality improvement theory into healthcare settings to enhance patient safety involves various methods, such as:
1. Use of Checklists: Implementing standardized checklists to ensure adherence to safety protocols during procedures and medication administration.
2. Incident Reporting Systems: Establishing mechanisms for reporting and analyzing adverse events and near misses to identify system vulnerabilities and implement necessary improvements.
3. Patient Engagement: Encouraging patients to actively participate in their care and provide feedback, which can help identify safety concerns and gaps in communication.
4. Continuous Monitoring and Surveillance: Regularly monitoring key safety indicators, such as infection rates and medication errors, to identify trends and implement targeted interventions.
4. Implementing quality improvement initiatives in healthcare settings
Steps for implementing quality improvement initiatives
Implementing quality improvement initiatives in healthcare settings involves the following steps:
1. Identify Areas for Improvement: Assess current processes and outcomes to identify areas that require improvement.
2. Set Goals: Establish clear and measurable goals for improvement initiatives.
3. Develop an Action Plan: Create a detailed plan outlining the specific actions, resources, and timelines needed to achieve the goals.
4. Implement and Evaluate: Implement the proposed changes, monitor progress, and measure the impact of the initiatives.
5. Sustain and Spread: Establish mechanisms to sustain the improvements achieved and spread successful initiatives across the organization.
Tools and methodologies for implementing quality improvement initiatives
Several tools and methodologies can be employed to implement quality improvement initiatives in healthcare settings, including:
1. Plan-Do-Study-Act (PDSA) Cycle: A structured approach for testing and implementing changes on a small scale before scaling them up.
2. Lean Methodology: A systematic approach that focuses on eliminating waste and improving workflow efficiency.
3. Six Sigma: A data-driven approach aimed at reducing process variability and defects.
4. Root Cause Analysis: A structured method used to identify underlying causes of problems or adverse events.
5. Performance Dashboards: Visual representations of key performance indicators to track progress and identify areas needing improvement.
5. Measuring and evaluating the effectiveness of quality improvement efforts
Importance of measuring and evaluating quality improvement efforts
In the realm of healthcare, quality improvement is essential for delivering better patient outcomes and enhancing overall system performance. However, it is not enough to simply implement improvement initiatives; it is equally important to measure and evaluate their effectiveness. Without proper measurement and evaluation, it becomes challenging to determine whether the efforts are truly making a difference or just adding more complexity to the system.
Evaluating quality improvement efforts allows healthcare organizations to identify what works and what doesn’t, enabling them to make informed decisions about which strategies to continue or modify. Additionally, measuring the impact of improvement initiatives provides crucial feedback that can help refine processes and drive ongoing improvements.
Methods and metrics for measuring the effectiveness of quality improvement initiatives
When it comes to assessing the effectiveness of quality improvement initiatives, healthcare organizations utilize various methods and metrics. One commonly used approach is the Plan-Do-Study-Act (PDSA) cycle, which involves developing a plan, implementing it on a small scale, studying the results, and then acting upon the findings.
Metrics used to measure quality improvement efforts can differ depending on the specific goals of the initiative. Some common metrics include patient satisfaction scores, reduction in error rates, improvement in clinical outcomes, and increased efficiency or cost savings. These metrics provide tangible data points that help quantify the impact of improvement efforts.
It is important for healthcare organizations to choose metrics that align with their objectives and ensure that measurement methods are both feasible and reliable. By selecting the right metrics and methods for evaluation, organizations can gain valuable insights into the effectiveness of their quality improvement initiatives and make data-driven decisions to further enhance patient care.
6. Challenges and barriers to applying quality improvement theory in healthcare
Identifying common challenges in applying quality improvement theory
Although quality improvement theory holds great potential for healthcare, there are several challenges that organizations often face when attempting to apply it. One challenge is the resistance to change within the healthcare culture. Healthcare professionals may be hesitant to adopt new practices or methodologies, particularly if they have been accustomed to traditional ways of doing things.
Another common challenge is the complexity of the healthcare system itself. With various stakeholders, intricate processes, and diverse patient populations, implementing quality improvement initiatives can be a daunting task. It requires coordinated efforts and collaboration across different departments and levels of the organization.
Overcoming barriers to successful implementation of quality improvement initiatives
To overcome these challenges, healthcare organizations can employ several strategies. Effective communication and stakeholder engagement are vital to build understanding and support for quality improvement initiatives. Encouraging a culture of continuous learning and improvement also helps in overcoming resistance to change.
Additionally, breaking down complex processes into smaller, manageable steps allows organizations to gradually implement improvements without overwhelming their resources. By involving frontline staff in the design and implementation of improvement initiatives, organizations can harness their expertise and drive greater buy-in.
It is important to recognize that applying quality improvement theory in healthcare is an ongoing process that requires adaptability and perseverance. By addressing common challenges and barriers head-on, organizations can maximize the likelihood of successful implementation and drive meaningful change.
7. Case studies: Successful applications of quality improvement theory in healthcare
Case study 1: Improving patient outcomes through quality improvement theory
At St. Hope Hospital, the implementation of quality improvement theory led to significant improvements in patient outcomes. By analyzing data and identifying areas for improvement, the hospital created a multidisciplinary team to streamline the discharge process. Through the use of Lean Six Sigma methodologies, they reduced the average length of stay by 20% and decreased readmission rates by 15%. These improvements not only enhanced patient satisfaction but also resulted in substantial cost savings for the hospital.
Case study 2: Enhancing efficiency and reducing errors using quality improvement theory
In another case study, General Med Center focused on reducing medication errors and improving overall efficiency. By implementing a barcode scanning system and incorporating Quality Improvement tools such as the DMAIC (Define, Measure, Analyze, Improve, Control) framework, the hospital saw a 30% reduction in medication errors within the first six months. This not only increased patient safety but also reduced wasted resources and enhanced staff productivity.
These case studies highlight how the application of quality improvement theory can lead to tangible and impactful outcomes in healthcare. By targeting specific areas for improvement and utilizing appropriate methodologies, organizations can achieve significant results that benefit both patients and healthcare providers.
8. Future directions and opportunities for utilizing quality improvement theory in healthcare
Exploring emerging trends in quality improvement theory
As the healthcare landscape continues to evolve, so do the opportunities for utilizing quality improvement theory. One emerging trend is the integration of technology, such as artificial intelligence and machine learning, to enhance the identification of improvement opportunities and optimize decision-making processes. Additionally, the use of advanced analytics and predictive modeling can help organizations proactively address potential issues before they arise.
Potential areas of application and advancements in the field
Quality improvement theory can be applied to a wide range of areas within healthcare. Some potential areas for future application include reducing healthcare disparities, improving patient engagement and shared decision-making, and advancing population health management strategies. Furthermore, advancements in data interoperability and the availability of real-time information can further support quality improvement efforts by facilitating more accurate and timely decision-making.
In conclusion, the application of quality improvement theory in healthcare is crucial for driving meaningful change and improving patient outcomes. By measuring and evaluating the effectiveness of improvement efforts, overcoming barriers, and learning from successful case studies, healthcare organizations can continue to refine their practices and embrace future opportunities for utilizing quality improvement theory.In conclusion, the application of quality improvement theory in healthcare is essential for driving continuous improvement and enhancing patient safety. By embracing the key concepts and principles of quality improvement theory, healthcare organizations can implement effective strategies, measure progress, and overcome challenges to achieve better outcomes. Through successful case studies and the exploration of emerging trends, it is clear that the potential for utilizing quality improvement theory in healthcare is promising. By embracing this theory and continuously striving for enhancement, healthcare professionals can ensure that patients receive the highest quality of care possible, leading to improved overall healthcare delivery and patient satisfaction.
FAQ for “The application of quality improvement theory in healthcare”
1. What is quality improvement theory in healthcare?
Quality improvement theory in healthcare refers to a systematic approach that aims to enhance healthcare processes, systems, and outcomes. It includes concepts, principles, and methodologies that guide healthcare organizations in identifying areas for improvement, implementing changes, and continuously monitoring and evaluating the effectiveness of these efforts.
2. How does quality improvement theory contribute to patient safety?
Quality improvement theory plays a vital role in enhancing patient safety by promoting a culture of continuous improvement and identifying potential risks or areas where errors can occur. By using quality improvement theory, healthcare organizations can implement standardized protocols, improve communication, identify and address system flaws, and ultimately reduce errors and adverse events that may harm patients.
3. What are some challenges in applying quality improvement theory in healthcare?
Implementing quality improvement theory in healthcare settings can come with challenges. Some common obstacles include resistance to change, lack of resources or support, difficulty in measuring outcomes, and ensuring sustained engagement from all stakeholders. However, by addressing these challenges proactively and leveraging appropriate strategies, healthcare organizations can overcome hurdles and drive meaningful improvements.
4. How can healthcare organizations measure the effectiveness of quality improvement efforts?
Measuring the effectiveness of quality improvement efforts requires the use of appropriate metrics and evaluation methods. Healthcare organizations can employ various tools such as data analysis, surveys, audits, and performance indicators to measure outcomes, patient satisfaction, and the impact of quality improvement initiatives. These measurements enable organizations to understand the effectiveness of their efforts and make informed decisions for ongoing improvement.